Impact of Proposed Revision to Annex 1 on Disinfection in the Manufacture of Sterile Medicinal Products
Impact of Proposed Revision to Annex 1 on Disinfection in the Manufacture of Sterile Medicinal Products
Abstract
The proposed revision to Annex 1 has seen a number of significant changes with one of the main points being that a contamination control strategy based on principles of Quality Risk Management (QRM) is implemented across the facility which focusses on contamination control holistically. This additional requirement has resulted in the introduction of several new sections and enhancements to existing sections and requirements. The section on sanitation has been completely rewritten and is now referred to as Disinfection with significant enhancements to the individual clauses. This paper provides a review of these enhanced requirements for disinfection as well as the factors to consider during risk assessments of disinfection processes. In addition, this paper includes an informative review of the test methods associated with Disinfectant Efficacy Testing and how environmental monitoring data should be used to verify the ongoing effectiveness of disinfection processes.
Introduction
Disinfection is a crucial aspect of the control process but should not be considered as a stand-alone element. Historically, disinfectants were often chosen purely on the basis of their bactericidal effect on compendial organisms exposed to the agent in a test tube. i.e. a laboratory suspension test.

The expectation of Regulatory Authorities has changed considerably and a much more in depth approach in developing a robust disinfection regime is required. Consideration should be given to component parts constituent of the entire manufacturing process with respect to disinfection. This often requires the use of process flow diagrams to determine disinfection steps and the use of risk assessment tools like HACCP or RMC to verify that contamination hazards have been identified, transfer routes for contamination have been understood and verify that suitable control measures are in place.
It is clear throughout the revised Annex 1 that Risk Assessment is at the forefront of the decision making process. It is cited repeatedly throughout the document and is of the utmost importance when developing a strategy for a holistic approach to disinfection control.
Developing a Disinfection Regime
If we are to consider a new pharmaceutical manufacturing facility it is clear that a disinfection regime can be developed logically and systematically, carefully considering the risks involved throughout.
During this risk assessment process, there is scope to carefully consider disinfectant types, formulations, modes of action, efficacy, intended use, fitness for purpose etc.
However, many manufacturing facilities inherit their disinfection regime where modifications are made on an ad hoc basis when needs must. This is not an ideal scenario but constraints resulting from operational needs often preclude an in depth review and change to the disinfection process. As previously mentioned however, a comprehensive review of the disinfectant regime is currently an expectation of the regulatory authorities.
As a precursor to disinfection, a cleaning stage is usually included in the process (the degree of cleaning is dependent on the level of soiling). Cleaning is an important consideration for a number of reasons and the following aspects should certainly be considered:
- The presence of organic soiling: The action of disinfectants is diminished when used on soiled surfaces: they should be cleaned prior to disinfection.
- Compatibility of the cleaning agent with the disinfectant: Some cleaning agents leave residues which can adversely affect the disinfectant. The compatibility with the disinfectant or the removal of residues should be demonstrated practically. Cleaning Validation or alternatively Disinfectant Efficacy Testing (D.E.T) in the presence of cleaning agent residues are methods of choice.
The number and type of disinfectant agent should be considered including the use of a suitable sporicidal agent. Additionally, cleaning agents used prior to disinfection are recognised as part of the regime. The rationale for disinfection selection, rotation, site and frequency of use is less well documented in Annex 1.
It is incumbent on the end user to determine the frequency of use; rotation of and specific defined use of these agents to achieve optimum results. The review of Environmental Monitoring trend data is essential and should form an integral part of the exercise.
Disinfectant Efficacy Testing (D.E.T.)
A number of laboratory tests exist to determine the efficacy and suitability of a disinfectant. The appropriateness of the test is determined by the scope and/or intended use. Examples of items that may need to be disinfected include shoes; garments; gloved/ungloved hands; equipment; machinery; wrapped filling components; facility surfaces, water systems and air handling units. Clearly one disinfectant and one D.E.T method will not serve all purposes.
Suspension tests1 are valuable indicators when assessing relative efficacy. The environmental flora in clean rooms should be regularly assessed for susceptibility to the in use disinfectant. Suspension tests can be a useful starting point and may be used as an aid in disinfectant selection. Without too much difficulty a number of disinfectants can be screened to determine the relative resistance of both typed strains and environmental isolates. The tests should serve only to compare disinfectants with similar modes of action and may form a basis for optimising disinfectant choice. Ultimately, cost benefits may be gained by screening disinfectants using a suspension method as full surface D.E.T is a time consuming exercise. However, it should be noted that suspension testing is not an appropriate method to assess bactericidal / fungicidal activity for a defined use. (e.g. disinfection of a stainless steel surface with a given agent, a prescribed contact time and set temperature range)
End users should be aware that when qualifying sporicidal disinfectants, the suspension test is often used by disinfectant manufacturers. Manufacturers label claims can be easily misinterpreted as C’s of A often mix and match suspension and surface testing results.
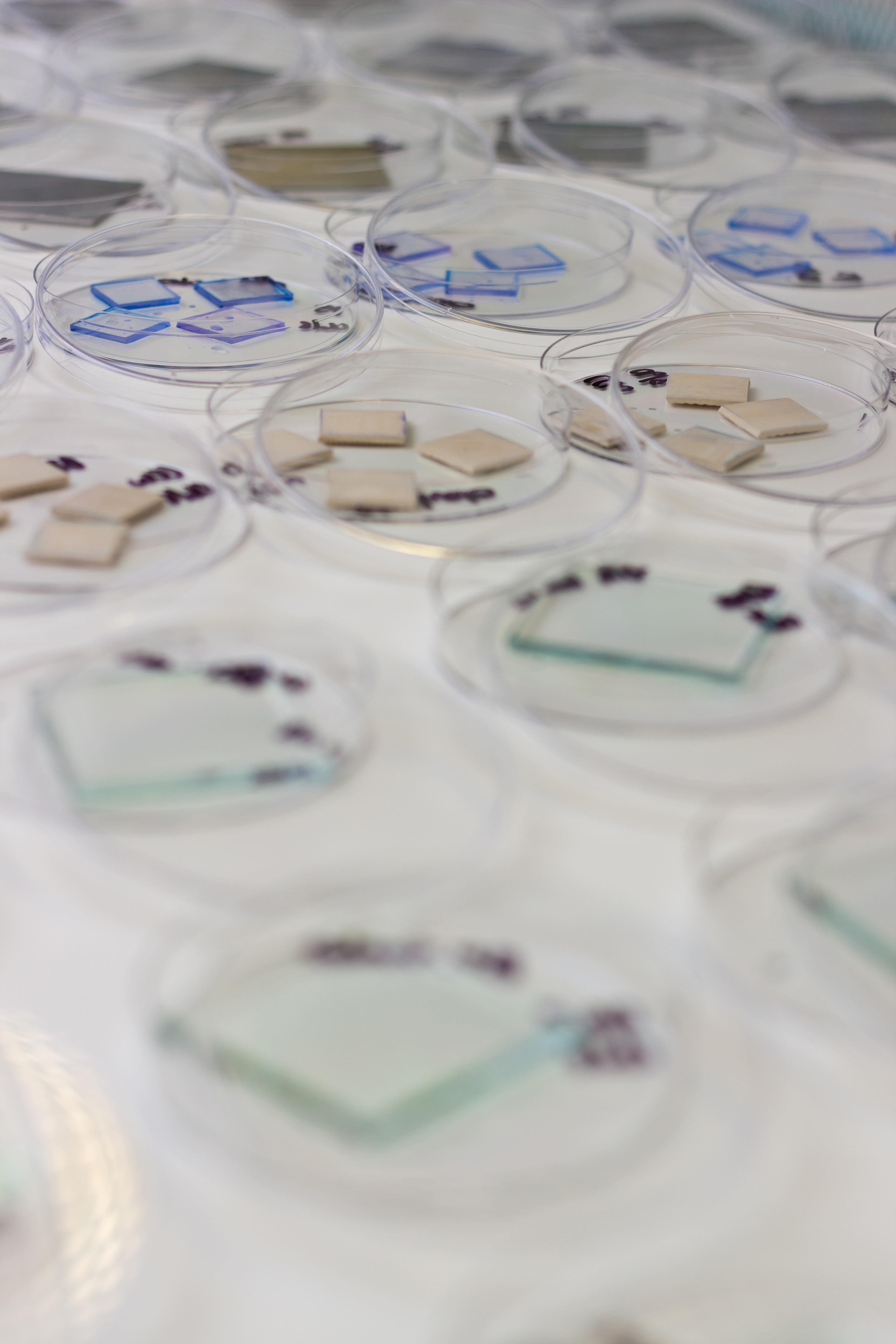
Surface Testing of Disinfectants
Validation of disinfectant efficacy, mimicking operational use is proposed in the Annex 1 revision. It is likely that the majority of pharmaceutical manufacturers currently adopt this approach but shortly it is expected to become an expectation according to the new GMP guidelines described in Annex 1. The U.S.P.2 currently describes the need for a surface test and BS EN 136973 analysis is the method of choice to satisfy European requirements with respect to surface testing. It is notable that the scope of BS EN 13697 does not include surface testing of disinfectants against spores.
Surface testing should encompass a range of representative surfaces, contact times and micro-organisms such that worst case operational conditions are most closely imitated, in this way meaningful results are achieved. The most prevalent and latest environmental isolates should be included in D.E.T. when the relative resistance of these isolates can be measured. This is especially true for isolates from higher grade areas and for spore forming organisms where it is clearly critical that the continuing efficacy of in use disinfectants is demonstrated. D.E.T. should be viewed therefore as a dynamic process and not a one off exercise.
Shelf-Life of Disinfectants:
In the revision to Annex 1 it is proposed that the efficacy of a disinfectant be demonstrated throughout its shelf life “ 5.33 Disinfectants should be shown to be effective for the duration of their in-use shelf-life taking into consideration appropriate contact time and the manner in and surfaces on which they are utilised.”4
The user of the disinfectant may need to consider the expiration date for the disinfectant and have some data to show the efficacy of the disinfectant at the end of its shelf life or beyond the expiry date. The initial DET validation work may not have included shelf life studies and this may be an area for users to reassess.
The shelf-life of a disinfectant should be determined empirically, clearly defined and should relate to efficacy testing of the agent and include the most resistant micro-organisms for that class of disinfectant.
Bioburden of Disinfectants:
Disinfectants used in grade A and B areas should be sterile, and those used in lower grade areas should have a predetermined bioburden limit. There is a need therefore to submit samples of in use disinfectants for laboratory analysis to assess the bioburden. This should be done at a defined frequency and on stipulated occasions throughout the shelf life, including start and end of shelf-life.
D.E.T. Acceptance Criteria for Surface Testing:
The USP includes an expectation that surface challenge tests must show a 2 log reduction for spores and a 3 log reduction for vegetative bacteria.
BS EN 13697:15 characterises bactericidal activity by a 4 log or more reduction in viability for Pseudomonas aeruginosa, Staphylococcus aureus, Enterococcus hirae and Escherichia coli (under defined conditions). Fungicidal activity is characterised by a 3 log reduction or more reduction in viability for Candida albicans and Aspergillus brasiliensis.
As it may be seen above, various criteria exist depending on the regulator. It may be prudent to adapt the acceptance criteria of the generic norms to represent the use of the disinfectant within a specific pharmaceutical facility. The defined target log reduction should be based on the facility bioburden. It must be remembered however that the efficacy of a disinfection programme can only truly be judged by review of environmental monitoring trend data5.
Summary and Conclusion
Whilst the need for Disinfectant Efficacy Testing, remains a critical aspect of contamination control, the emphasis is shifting towards a greater need for risk assessment in the proposed revision to Annex 1. Manufacturers will have to have a well thought out contamination control strategy in place which includes consideration for disinfection steps in the process. In existing facilities and processes the use of disinfectants and the effectiveness may need to be reassessed to ensure that the appropriate laboratory testing was performed, that the original DET testing included in house environmental flora and that a system is in place to allow the ongoing assessment of new environmental isolates into the disinfection regime.
About the Author
Author: Denise Irving
Denise Irving works as a Senior Microbiology Consultant at the Honeyman Group. With over 30 years of experience in the pharmaceutical industry, Denise has performed countless contamination strategies using tools such as HACCP and has developed microbiological methods for Disinfectant Efficacy Testing at Honeyman.
Honeyman have worked with many clients to verify that the in-use disinfectant was effective and suitable for use the process. We have experience of the standard suspension and surface tests defined in the ISO standards. On many occasions have been able to develop bespoke methodology which is representative of the in house cleaning and disinfection regime used by the client in their facility.
For further information regarding Disinfection Efficacy Testing, see our dedicated DET page on the Laboratory site or contact a member of the Honeyman Group Laboratories team to discuss your specific requirements.
Email enquiries@honeymangroup.com or phone +44(0) 1833690101
Bibliography:
1) Suspension Tests:
BS EN 1040: Chemical disinfectants and antiseptics – Quantitative Suspension test for the evaluation of basic bactericidal activity of chemical disinfectants and antiseptics – Test methods and requirements (Phase 1).
BSEN 1275: Chemical disinfectants and antiseptics – Quantitative Suspension test for the evaluation of basic fungicidal or basic yeasticidal activity of chemical disinfectants and antiseptics – Test methods and requirements (Phase 1).
BS EN 1276: Chemical disinfectants and antiseptics – Quantitative Suspension test for the evaluation of basic bactericidal activity of chemical disinfectants and antiseptics used in food, industrial, domestic and institutional areas. Test method and requirements (Phase 2 – Step 1).
2) USP version 40 General Chapter <1072> Disinfectants and Antiseptics – Disinfectant Challenge Testing.
3) BS EN 13697 Chemical disinfectants and antiseptics – Quantitative non-porous surface test for the evaluation of bactericidal and/or fungicidal activity of chemical disinfectants used in food, industrial, domestic and institutional areas. Test method and requirements (Phase 2 – Step 2).
4) Eudralex volume 4 – Good Manufacturing Practice Guidelines
(Annex 1 “Guide for the Manufacture of Sterile Medicinal Products”).
5) PHSS publication: Bio-contamination (Section 3.0 PHSS Technical Monograph No.20)
Download the PDF: Impact of Proposed Revision to Annex 1 on Disinfection in the Manufacture of Sterile Medicinal Products
© Honeyman Group 2018
Our Customers: